EMDR (Eye Movement Desensitization and Reprocessing)
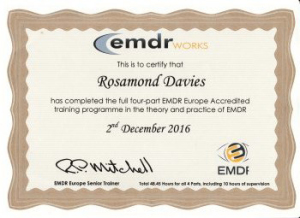
I am a qualified EMDR therapist. EMDR is recognised by The World Health Organisation and recommended in NICE guidelines as the preferred treatment for Trauma and PTSD.
Trauma and EMDR
What is Post Traumatic Stress (PTS)
PTS is a collection of reactions – feelings, thoughts, behaviours – which are experienced following a sudden distressing event which is outside the range of normal everyday human experience. The experience is overwhelming and exceeds our normal ability to cope. It is the unexpectedness of the incident which seems to evoke the stress because it undermines our trust in normality – we can never quite believe in an ordered existence any more.
Typical examples of traumatic events include
- Natural disasters
- Accidents
- Sexual or physical assaults
- Terrorist attacks
- Combat during wartime
During a traumatic event, we think that our life or the lives of others is in danger. We feel afraid or feel that we have no control over what is happening. Combat-related PTSD has existed as long as war itself. The condition was called “Shell Shock” in World War I, and “Combat Fatigue” in World War II. Despite the fact that the condition has been around for thousands of years, it is sometimes still difficult, or controversial, to diagnose.
PTS symptoms may not be experienced for days, weeks or even months after the event and can affect us even if we are not directly involved in the incident. E.g. We may witness the accident, be a rescue worker or have friends or relatives who are involved.
PTS symptoms are a normal short-lived response to trauma . They act as a way of helping our mind and body to process the event and to try to make sense of it, so that we can eventually react to it in a less distressing way. It is thought that about 20% of people who suffer Post Traumatic Stress go on to develop Post Traumatic Stress Disorder (PTSD). It is only when the symptoms persist after several months that Post Traumatic Stress becomes Post Traumatic Stress Disorder.
Signs and Symptoms
Generally, symptoms of PTSD can be like re-experiencing the traumatic event or are experiencing high levels of anxiety related to the event. These symptoms are made even more distressing as they can occur at any time and we have no control over them. No wonder we try to avoid thinking about the event by any means we can create. Some of the most common symptoms include:
- Having recurrent nightmares.
- Acting or feeling as though the traumatic event were happening again, sometimes called a “flashback”.
- Being physically responsive, such as experiencing a surge in our heart rate or sweating, when we think of the traumatic event.
- Having a difficult time falling or staying asleep or wanting to sleep all the time as a way of switching off.
- Feeling more irritable or having outbursts of anger.
- Feeling constantly “on guard” or as if danger is lurking around every corner (Hypervigilance).
- Making an effort to avoid thoughts, feelings or conversations about the traumatic event and avoiding activities and / or places which arouse recollections of the event.
- A loss of interest in important, previously positive, activities.
- Experiencing difficulties having positive experiences such as happiness or love.
- A sense of being vulnerable leading to a fear of losing control.
- Survivor guilt.
- Changes in feeling about ourselves (E.g. feeling useless).
- Numbed responses.
- Reduced interest in the external world – feeling detached and estranged.
- Forgetting important parts of the event or being unsure if memories are real or imagined.
The reason we cannot control PTSD is because it causes changes in the brain. The good news is that with the right help we can reverse those changes and begin to enjoy life again.
What follows is a very simple explanation of the changes that occur in the brain and should help to explain just why we are unable to simply ‘pull ourselves together’ and get on with life as we used to.
How Trauma Changes The Brain
The Triune Brain model, introduced by physician and neuroscientist Paul D. MacLean, explains the brain in three parts:
- Reptilian (brain stem): Often described as the primitive brain is the innermost part of the brain and is responsible for survival instincts and autonomic body processes. (fight, flight or freeze response)
- Mammalian (limbic, midbrain): The midlevel of the brain, this part processes emotions and conveys sensory relays.
- Neommalian (cortex, forebrain): The most highly evolved part of the brain. This area controls our thinking and reasoning, decision-making, learning and memory.
During a traumatic experience, the reptilian brain takes control, shifting the body into reactive mode. The only thing that concerns us is our survival. We don’t think of the beautiful colour of the lions eyes or wonder what it weighs as it bounds towards us. The thinking part or our brain (Neocortex) switches off and the brain stem orchestrates survival mode. At this time the sympathetic nervous system increases stress hormones and prepares the body for the fight, flight or freeze response.
Hopefully, when the immediate threat ceases, (the lion is darted and dragged away) the parasympathetic nervous system shifts the body into restorative mode. This process reduces stress hormones, we realise the danger is over and the Neocortex (reasoning part of the brain) is switched back on. Ideally this occurs soon after the trauma or within hours or days.
However, for those 20 percent of trauma survivors who go on to develop symptoms of post-traumatic stress disorder (PTSD) the shift from reactive to responsive mode never occurs. Instead, the reptilian brain, which has no sense of time and is geared to the Fight, Flight or Freeze, continues to hold the survivor in a constant reactive state. The experience cannot be stored as a memory but continues to hold its distressing emotional charge.
In the brain several chemical and biological imbalances can present after trauma. Their effects are especially exacerbated by three major brain function dysregulations:
- Overstimulated Amygdala: An almond-shaped mass located deep in the brain, the Amygdala is responsible for survival-related threat identification, plus tagging memories with emotion. After trauma the Amygdala can get caught up in a highly alert and activated loop during which it looks for and perceives threat everywhere.
- Underactive Hippocampus: An increase in the stress hormone glucocorticoid kills cells in the Hippocampus, which renders it less effective in making synaptic connections necessary for memory consolidation. This interruption keeps both the body and mind stimulated in reactive mode as neither element receives the message that the threat has transformed into the past tense.
- Ineffective variability: The constant elevation of stress hormones interferes with the body’s ability to regulate itself. The sympathetic nervous system remains highly activated leading to fatigue of the body and many of its systems, most notably the adrenal.
How Healing Happens
While changes to the brain can seem, on the surface, disastrous and representative of permanent damage, the truth is that all of these alterations can be reversed. The Amygdala can learn to relax; the Hippocampus can resume proper memory consolidation; the nervous system can recommence its easy flow between reactive and restorative modes. The key to achieving a state of neutrality and then healing lies in helping to reprogramme the body and mind.
What is Eye Movement Desentisation and Reprocessing (EMDR) and how does it work?
EMDR is an acronym for ‘Eye Movement Desensitisation and Reprocessing’. EMDR is a powerful psychological treatment method for PTSD and phobias that was developed by an American clinical psychologist, Dr Francine Shapiro, in the 1980s. As a Senior Research Fellow at the Mental Research Institute, she published the first research data to support the benefits of the therapy in 1989.
Because EMDR is a complex and powerful therapy, therapists always have a background in mental health before undertaking EMDR training. EMDR is a recognised and recommended treatment for PTSD by the World Health Organisation and forms part of NICE guidelines nice.org.uk/guidance/cg26
EMDR helps a person see disturbing material in a new and less distressing way. Put simply, EMDR mimics what occurs naturally during dreaming or REM (rapid eye movement) sleep. During this stage of sleep, our minds are busy trying to process our experiences.
EMDR has a direct effect on the way the brain processes information, restoring a healthy connection between the limbic brain and the Neocortex so that normal information processing is resumed and traumatic experiences can be located in the past and no longer impact on the present. Following a successful EMDR session, we no longer relive the images, sounds and feelings when the event is brought to mind. We still remember what happened, but it is less upsetting.
EMDR for treating Phobias
Phobias take many forms such as Agoraphobia, Claustrophobia, heights, spiders, snakes, flying, needles etc. We can develop phobias about just about anything. Most phobias have their roots in childhood brought on by a traumatic event that we have been unable to process. They can also develop in adulthood. We recognise that our fear is excessive and not entirely rational but are unable to control it. Phobias can severely limit a person’s life and create great distress. EMDR can be an extremely effective in treating phobias and anxieties.
Please note:
EMDR is not a quick fix but involves a great deal of commitment and hard work. We will need to get to a place where you feel you can trust me and feel relaxed enough to be completely open and honest. There is a great deal of preparation involved, including taking a detailed chronological history of all past traumatic experiences and working on developing effective coping and self-soothing methods which are geared to your individual needs before we can start to process the trauma or phobia.